Our health industry expert and managing director, Kalen Stanton, continues this blogcast (podcast + blog), In Light of Change, and builds further on the why of change. In this episode, Vanderbilt Health leaders share insight on how to inspire and engage your clinical teams to deliver personalized patient care. Below is a summary of the episode – featuring Dr. Paul Sternberg, Chief Medical Officer and Brian Carlson, Senior Director of Patient Experience at Vanderbilt Health.
What you’ll hear:
- Words matter: how Vanderbilt defines clinician (vs. provider)
- Why physicians often feel marginalized
- How to get your clinicians’ attention in the right way at the right time
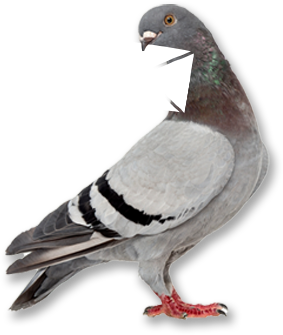
- The four Roots of Engagement apply to clinicians too
- Immediate next steps to apply in your health organization
Listen to the full conversation here.
HOW TO ENGAGE A CLINICIAN
Kalen: I’m excited to start by discussing the definition of clinician in the health space. How do you define it at Vanderbilt?
Paul: From my perspective as a physician, a provider is a business term. It takes away the special relationship you develop as a caregiver. And so we prefer to be called either a doctor or clinician. It’s similar to my feeling that we should call the people receiving care patients and not consumers. There is a difference. A patient has an issue that differentiates them from the conventional consumer. And although there may be consumer principles that can be applied to their care and there can be business principles that can help us in our roles as caregivers, there needs to be a distinction. That’s why I like the terms patient and clinician to be used.
PHYSICIANS FEEL MARGINALIZED
Kalen: What have the two of you found to be the most crucial points of discussion regarding how we personalize the experiences of our patients?
Paul: I would start by saying that when a patient makes a decision about where they’re going to get their care, it is primarily driven by which doctor they want to go to. Now, they may have an emergent situation where they choose a hospital emergency room, but for most of us, we initiate our entry into the health care system for a clinical problem by selecting a physician. And the physicians know that, but then they look at what’s going on in the health care world and see all these decisions being made by administrators that are not including them in that process. Our physicians feel marginalized. And they are the ones that are at the front line – along with nurses. And I think a lot of nurses feel the same way. One thing Brian and I have tried very hard to do at Vanderbilt is to identify ways we can listen to our caregivers and involve them. Some of it is just educating them about the decisions that are being made so they know what’s happening.
Brian: I completely agree. Also recognizing that health care is a team sport. It’s not just the clinician, but there are many people surrounding that clinician who are part of the team that clinician is relying upon. All of those people together make that experience. In order to change the experience, we have to understand their experience. And that starts with getting to know them on their turf, on their terms. What are the pains that they feel, what are the successes they feel, and then – speaking as an administrator – how can we help them become more effective in their jobs and make their jobs easier?
Paul: Clinicians need to feel that the administrative leadership is there to enhance their ability to provide care.
SEEKING THE CLINICIAN’S ATTENTION
Brian: I think this is a good time to discuss what we’ve done to get our clinicians’ attention. Given their busy day and the enormous amount of information and data, not only for the patient, but also the institutional and professional priorities they are managing, what can be done to capture their attention?
Paul: I used to think that to get their attention, I had to elevate the email or the message to the highest authority. So they may not listen to me, but maybe they’d listen to the dean or the CEO. Well, it turns out that actually they’re more likely to read an email if it comes from someone lower in the org chart, such as their division chief, their medical director, or the person who manages their clinic. The higher it goes, the less likely they are to listen.
Brian: They also want it short, concise with the why. Why is this important? Not just do this, but what does this mean? What is the significance of what you’re asking me to do? And put that information right at the top.
WHAT’S GETTING IN THE WAY OF YOUR WHY?
Kalen: I feel like a lot of the conversations today are about how peoples’ whys are getting jumbled up with the hundred other things that are coming at us. The technologies, the processes, the to-dos, the check boxes, and so on. A lot of times we’re resisting changes because the how to get things done is getting in the way of the why we are here in the first place. I know you’ve created groups at Vanderbilt to tackle this conversation.
Paul: Yes, we have a physician’s council made up of the drivers of our clinical enterprise. This council has existed for 10 years now. We meet to discuss topics that we think are meaningful to them but will also provide insights to us. It’s been a great way to ensure this important group understands how their work influences (or can cause problems) for other areas of the organization.
A few years ago we realized we needed to involve another group in our council – younger doctors who are a large component of the organization and think differently. Because the doctors in their 30s or 40s may have different priorities or insights than doctors in their 50s and 60s, we created an early career physician council. They had to be in practice five years or less.
Brian: The younger council is also very interested in receiving mentoring . . . the importance of mentoring and what mentoring means to them earlier in their career.
Paul: And that’s not all. We also meet quarterly with various leaders in the middle – medical directors and division chiefs. They are a direct line to your front line. We like to have discussions around real issues. We’ll break folks up into small groups with a problem to solve. Let’s say, how to handle emergency room overcrowding, but not in the context of we need to build a bigger ER or we need additional MRI machines, but here is your space and equipment and staff. How are you going to enhance the patient experience with these existing factors and/or constraints? Then give them 20 minutes to brainstorm and report back on their ideas. This engages the group, helps them learn, and lets them feel like they’re a part of the solution.
THE FOUR ROOTS OF ENGAGEMENT
Readers: Listen to the audio to hear how Vanderbilt is doing on these four Roots of Engagement.
IMMEDIATE NEXT STEPS TO ENGAGING CLINICIANS
Kalen: What can other leaders in our audience do tomorrow to start leading clinician engagement?
Paul: Meet regularly with your clinician leaders to focus on what you can do for your doctors, physicians, etc. to keep them engaged, get them excited, and keep them informed.
Brian: You need to help them understand that in their role as clinicians, they are leaders of the care teams. The clinicians must realize their behavior to the staff around them is as important as their behavior to their patients. Clinicians need to think, “When I’m having a bad day, how do I act? How do I treat you? Do I say hello in the morning?” Their teams are modeling their behaviors.
Paul: To encourage engagement, you need to get people together to talk and connect. It’s a great idea to invite a non-physician facilitator to keep the conversation on track, make sure everyone provides input, and ask thoughtful questions as a sophisticated outsider. Leading yourself is not as effective.
Brian: As a leader, make sure you’re out and around gathering intelligence so you have a strong pulse and accurate picture of the challenges facing your organization to be prepared in your next conversations. You can do this by attending meetings or listening to one-on-one conversations in your surrounding. Don’t isolate yourself in your office.
Ready to engage your clinicians, or are you interested in how Root approaches this critical focus area in strategic change? Send Kalen and the team a note here to continue the conversation on engaging your team in the future of health transformation.